World Health Day - ‘depression, let’s talk’
WORLD Health Day, celebrated on 7 April every year to mark the anniversary of the founding of the World Health Organisation (WHO), provides an unique opportunity to mobilise action around a specific health topic of concern to people all over the world.
The theme of 2017 World Health Day campaign is “depression - let's talk”.
Depression affects people of all ages, from all walks of life, in all countries. It causes mental anguish and impacts on people's ability to carry out even the simplest everyday tasks, with sometimes devastating consequences for relationships with family and friends and the ability to earn a living. At worst, depression can lead to suicide, now the second leading cause of death among 15 to 29-year-old people.
Yet, depression can be prevented and treated. A better understanding of what depression is, and how it can be prevented and treated, will help reduce the stigma associated with the condition, and lead to more people seeking help.
Living with someone with depression can be difficult. Here are some tips on what to do to help someone you live with who is depressed, while taking care of yourself at the same time.
What you should know
- Depression is an illness and not a character weakness.
- Depression can be treated. What treatment is best and how long the depression lasts depend on the severity of the depression.
- The support of carers, friends and family facilitates recovery from depression. Patience and perseverance is needed, as recovery can take time.
- Stress can make depression worse.
What you can do for people who are depressed:
- Make it clear that you want to help, listen without judgement, and offer support.
- Find out more about depression.
- Encourage them to seek professional help when available. Offer to accompany them to appointments.
- If medication is prescribed, help them to take it as prescribed. Be patient; it usually takes a few weeks to feel better.
- Help them with everyday tasks and to have regular eating and sleeping patterns.
- Encourage regular exercise and social activities.
- Encourage them to focus on the positive, rather than the negative.
- If they are thinking about self-harm, or have already intentionally harmed themselves, do not leave them alone. Seek further help from the emergency services or a health-care professional. In the meantime, remove items such as medications, sharp objects and firearms.
- Take care of yourself too. Try to find ways to relax and continue doing things you enjoy.
Life changes which come with aging can lead to depression - to prevent and treat the elderly:
- Depression is an illness characterised by persistent sadness and a loss of interest in activities that you normally enjoy, accompanied by an inability to carry out daily activities, for at least two weeks.
- In addition, people with depression normally have several of the following: a loss of energy; a change in appetite; sleeping more or less; anxiety; reduced concentration; indecisiveness; restlessness; feelings of worthlessness, guilt, or hopelessness; and thoughts of self-harm or suicide.
- Depression among older people is often associated with physical conditions, such as heart disease, high blood pressure, diabetes or chronic pain; difficult life events, such as losing a partner; and a reduced ability to do things that were possible when younger.
- Depression is treatable, with talking therapies or antidepressant medication or a combination of these.


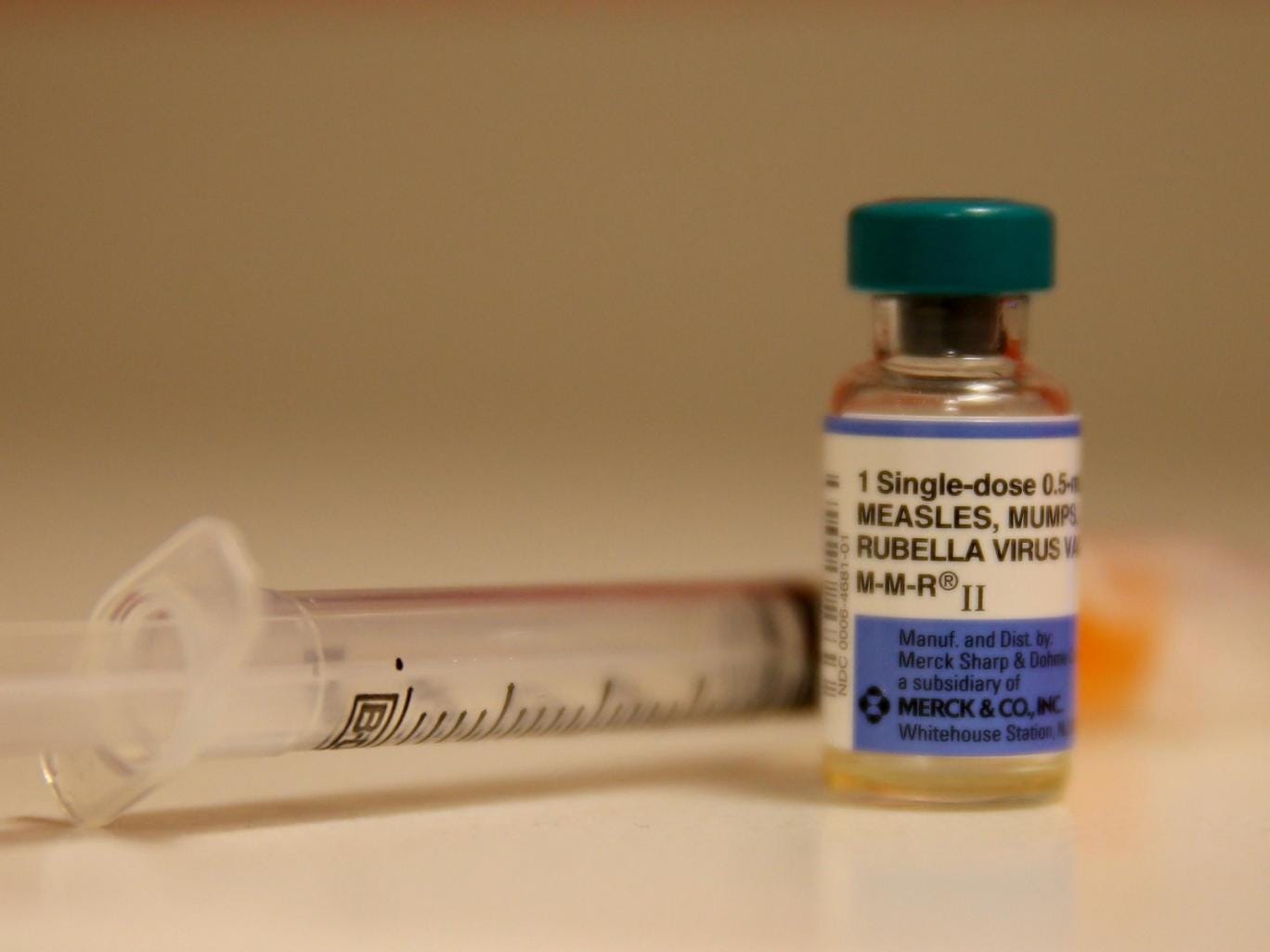 Major measles outbreaks are spreading across Europe despite the availability of a safe, effective vaccine, the World Health Organisation has warned.
Major measles outbreaks are spreading across Europe despite the availability of a safe, effective vaccine, the World Health Organisation has warned. The number of people developing and dying from tuberculosis (TB) is falling in Europe, but among the most vulnerable — including migrants, prisoners and people who are HIV positive — there have been worrying increases, data showed on Monday.
The number of people developing and dying from tuberculosis (TB) is falling in Europe, but among the most vulnerable — including migrants, prisoners and people who are HIV positive — there have been worrying increases, data showed on Monday.